
Did you know the estimated number of combat service members, veterans who suffer from signature wounds such as invisible injuries of combat trauma, traumatic brain injury (or both) is 1 in 3? These signature wounds include painful symptoms such as flashbacks, avoidance, isolation, hyper-arousal reactions including anger outbursts. Operation Red Wings Foundation’s focus is to educate service members, veterans and their family members on the warning signs, symptoms, and characteristics of these injuries to better prepare our men and women when returning home.
Today, there are many terms to describe combat trauma, Post-Traumatic Stress Disorder (PTSD)
and Operational stress. These struggles are what many servicemen and women deal with after exposure to life
threatening situations. Whether one witnesses, or is directly involved with the event, it can have
profound psychological effects on the individual.
Spouses and children can be greatly affected by these invisible injuries and their side effects. How? A spouse may become a “caregiver” and have to abandon the role as wife or husband, in order to deal with the daily crisis resulting from untreated PTSD, while a child, whose parent has PTSD, may develop anxieties and self-esteem issues.
Mild Traumatic Brain Injury (mTBI) and post-concussive disorder are terms used to describe head
injuries most experienced by service members, veterans. Injuries from mTBi, like PTSD, are not visible so the person does
not look injured. The symptoms are inconsistent. Sometimes your brain is working stronger, and you are okay, or
sometimes you struggle. Family members are the first to notice the changes and the first to fall victim to
the negative impact that comes with lack of diagnosis and treatment.
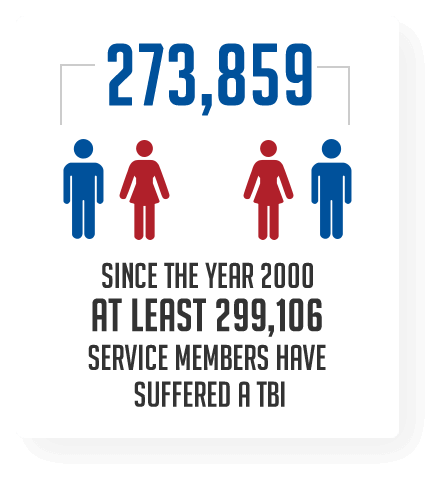
Mild Traumatic Brain Injury in SM is typically the result of direct blunt trauma to the head or blast injuries. The resulting effects of these are displayed over the course of time. Anywhere from immediately after the injury or, they may begin to demonstrate the signs days or weeks after the injury. Some signs of mTBI are, being dazed, confused, or disoriented. A person does not have to lose consciousness to incur mTBI. Other signs include issues with memory, concentration, balance, blurred vision, sensitivity to light, speech, and mood changes. Historically, the effect of these brain injuries will be all encompassing of one’s life. As with PTSD, the individual, family, and work life all suffer as a result of the changes to the person’s capability, which is why education is a key factor. ORWF provides the tools for individuals to learn how to cope with mTBI, understand it, and make changes to adapt and get stronger.
Chronic Pain is experienced by approximately half of all servicemen and women returning from deployment. Although difficult to diagnosis due to the different sites of injury which are often internal and not visible, chronic pain can be the result of amputations, burns, spinal cord damage, nerve damage, and back injuries just to name a few. Blasts can create powerful pressure waves on the body, overtime this continued exposure could damage central nervous system tissue contributing to chronic pain. Adding to this is the likely hood of frustration and stress which can exacerbate pain.
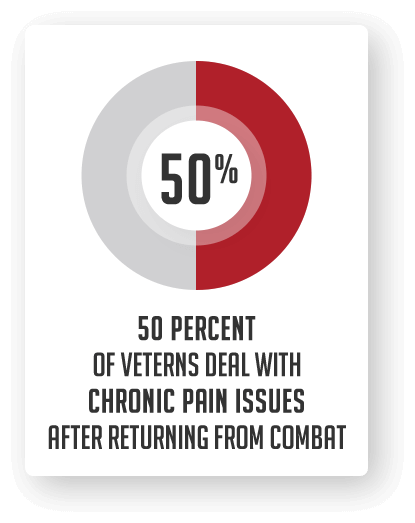
Spouses and family members, working on coping with their loved one’s chronic pain can be exhausting. The added pressure of “invisible pain” that is often not diagnosed by physicians can be extremely difficult and leave people feeling hopeless. There are new options and ongoing research treatments available for a variety of pain issues.
Military Sexual Trauma (MST) statistics vary and are judged to be under-reported by many, including
Defense Secretary Leon Panetta. The DoD estimates that of the 19,000 sexual assaults in the military in 2010, only 13% of
those were formally reported. The military laws for criminal acts, Uniform Code of Justice, differs greatly from US civilian
laws. Prosecution rates for sexual assault in the military is astonishingly low, 8%. An estimated 10% of alleged
perpetrators were allowed to resign instead of facing formal charges. The DoD does not maintain a sexual offender
registry as does the civilian legal system, which would alert commanders, military childcare programs,
etc. of the presence of a perpetrator in a particular community
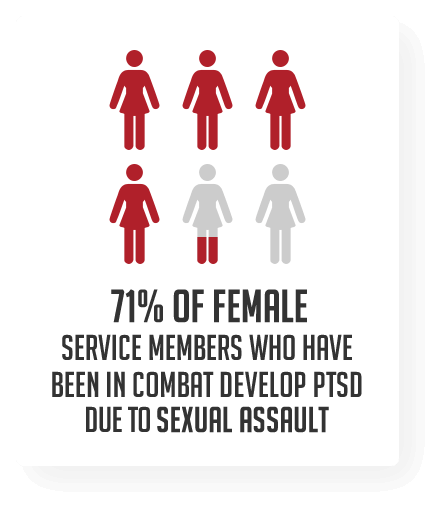
Post-Traumatic Stress Disorder (PTSD) is the common result of any sexual assault and within the military community the level of trauma is compounded. MST survivors face a long and painful recovery and need the support of the military community as well as the civilian community to overcome their psychological injuries.
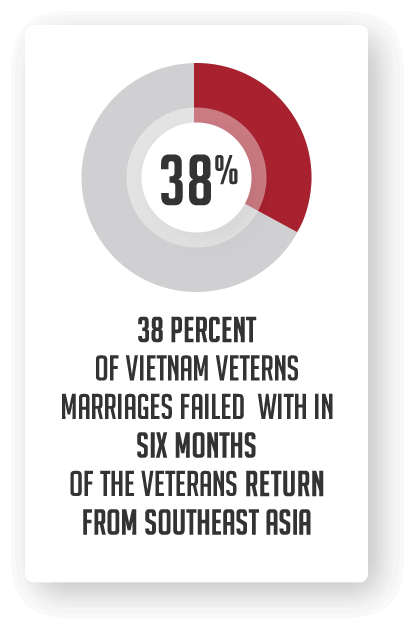
The stress on military families from overseas deployments is immense. When a service member is deployed, the separation can be lonely and difficult for both the service member and his or her spouse. As challenging as being apart can be, however, coming home often involves hard realities as well. This is especially the case when a spouse is severely injured. The pressure of coping with wartime injuries is often a cause of military divorce. The sheer number of soldiers who have returned from Iraq or Afghanistan suffering from Post-Traumatic Stress Disorder (PTSD) and other related problems is undeniable.
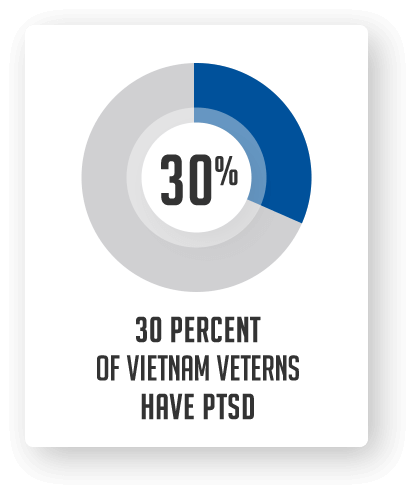
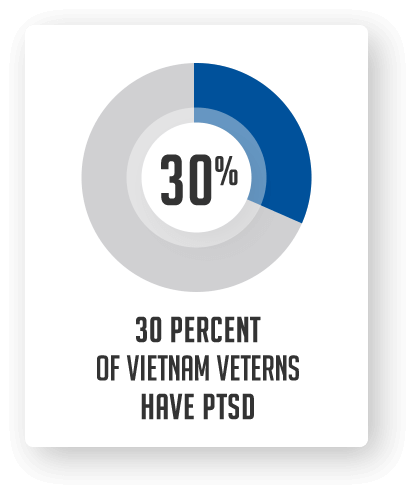
PTSD also takes a toll on marriages and other relationships. For example, research has found that 38 percent of “Vietnam veteran marriages failed within six months of the veteran’s return from Southeast Asia.” Research also finds that “veterans with PTSD are more likely to report marital or relationship problems, higher levels of parenting problems, and generally poorer family adjustment than veterans without PTSD.” A 2005 Pentagon study found that the divorce rate for Iraq and Afghanistan veterans was up 78 percent since 2003.
The Operation Red Wings Foundation is a Federal 501(c)(3) Non-Profit EIN: 27-1850918 Website and Contents
© 2023 Operation Red Wings Foundation. All Rights Reserved.
June 28 marks the 20th anniversary of Operation Red Wings.
Help us honor the fallen by serving Veterans who carry invisible wounds.
Thanks to Elite Transportation, every dollar is matched up to $20,000.
💙 Your gift = Double the impact